Abstract
Background:
Osteoarthritis (OA) is the most common degenerative joint disorder. Sufferers of this condition find that it impacts on the quality of their lives (QoL). Exercise is thought to be an important non-pharmacological approach for symptom management.
Aim and Objectives: The purpose of this systematic literature review was to examine the effectiveness of exercise (both land and water based), in improving the QoL of individuals with knee osteoarthritis.
Methods:
A systematic search was undertaken of AMED, The Cochrane Library, CINAHL, MEDLINE and PEDro along with the Google Scholar databases. The timing of these searches was from September to November 2014. Studies were selected based on pre-set eligibility criteria. Two independent reviewers appraised the selected studies using the PEDro scale and collaborated in order to establish a rigorous perspective on the quality of the research.
Results:
From 782 papers initially, 12 studies were included in the review; 10 high quality and 2 moderate quality primary studies and involving a total of 687 participants. The three most common outcome measures used were KOOS (Knee Injury and Osteoarthritis Outcome Score), Nottingham health profile and SF 36. There was strong evidence supporting exercise and physical activity as effective in improving the QoL for people with knee OA based on 8 high and 2 moderate quality studies. The review did not draw any conclusions on the effects of aquatic exercise on QoL due to conflicting evidence. Also noted was conflicting levels of significance under different exercise conditions; significant difference was high when exercise was compared to a non-intervention or education control group and less so when exercise was compared with drug therapies such as NSAID.
Conclusion:
Exercise and physical activity, either combined with appropriate drug therapies, or as a single intervention is effective on improving QoL in people with knee OA. However, the most effective exercise dose prescription, the individual aspects of a multicomponent programme, or the additional benefit of a home exercise and walking programme remain uncertain.
Introduction
Osteoarthritis (OA), a degenerative joint disease, is one of the most common musculoskeletal disorders and represents a major, global public health problem (Alkan et al., 2013). The cause of the disease remains unknown; however, current evidence suggests that it is a result of an interplay of intrinsic and extrinsic risk factors such as old age, female gender, ethnicity, genetic factors, obesity, previous trauma, repetitive use of joints and occupation, which lead to the development of the disease particularly in weight-bearing joints like the knee (Iwamoto et al., 2011). It presents with progressive structural alterations to the joint which includes loss of articular cartilage, osteophytes formation, muscle weakness, and ligamentous laxity (Bennell et al., 2012).
Knee osteoarthritis is the most commonly encountered type, affecting about 18% of women and 9.8% of men globally and its incidence is projected to double by the year 2020, largely due to increased obesity and old age (Johnson and Hunter, 2014; Akinpelu et al., 2009). The disease progression is usually slow and characterised by stiffness, pain, muscle weakness, joint instability and reduced physical functions such as difficulty in walking, stair climbing and squatting, moving from sitting to standing (Yilmaz et al., 2012; Heidari, 2011; Chaipinyo, and Karoonsupcharoen, 2009). In advanced stages pain becomes continuous, muscle atrophy and limb deformity result (Micheal et al., 2010). All such complaints give rise to physical disability which could ultimately lead to restrictions in QoL with time (Yilmaz et al., 2012).
Background and literature review
The burden of knee OA does not only include physical problems, but also high economic and social burden largely attributed to the effects of the disability, comorbid diseases, treatment expenses (Bitton, 2009; Woolf and Pfleger, 2003). It also brings with it detrimental psychological effects such as helplessness, coping difficulties and depression, all experienced at higher levels than the general population in people with the condition (Litwic et al., 2013; Cook et al., 2007).
QoL is described as a global construct which includes all aspects of life such as an individual’s perceived position within societal systems and in relation to their expectations and concerns. QoL is reported to be low in people with knee OA with a correlation existing between disease progression and QoL levels dropping significantly compared with other chronic diseases (Farr II et al., 2013; Alves and Bassitt, 2013). It is evidenced that people with OA experience major changes in daily life influenced by the severity of symptoms and impact on functional capacity, affecting their QoL (Chan and Chan, 2011; Egan and Mantes, 2010).
In recent years, QoL has become an important outcome in chronic conditions such as OA where health involving living with and managing one’s condition becomes important (Bernad-Pineda et al., 2014; Phillips et al., 2013; Hoptman et al., 2009). Although not fatal, patients with knee OA are at risk of developing cardiovascular disease due to obesity (Pietrosimone et al., 2014) which could be linked to physical inactivity resulting from chronic pain and restricted joint mobility. Thus, with a progressive disease of multiple risk factors and symptoms, with no known cure and management of patients depending on relief of symptoms, the importance of improving QoL as an endpoint for management needs to be emphasised (Kao et al., 2012; Dias CR et al, 2003).
Management of osteoarthritis has been a combination of different therapies of both pharmacological and non-pharmacological nature. In physiotherapy, a wide range of treatments including exercise and physical activity are used. The treatment of OA is focused on reducing physical disability, controlling pain while lessening the potentially harmful side effects of medicines (Beckwee et al, 2009; Zhang et al., 2007). Exercise is considered as an effective conventional therapy for knee OA symptoms (Fransen and McConnell, 2008). Based on the evidence of a systematic review of guidelines for physical management of osteoarthritis, exercise was among the strongest recommended interventions as first choice conservative treatment particularly for knee OA (Beckwee et al, 2009; Hootman et al., 2003; Larmer et al., 2014; Royal Australian College of General Practitioners, 2009; Veenhof et al., 2012 and Zhang et al., 2008). Systematic reviews have established the benefits of exercise and physical activities in patients with knee OA on outcomes of pain and function (Smith et al., 2014a; Smink et al 2011., Zhang and Jordan, 2010; Fransen and McConnell, 2009a; Fransen and McConnell, 2008b). However, the effects of exercise and physical activity on QoL are not well established and no review undertaken to date.
Primary studies have assessed the effectiveness of exercise and physical activity on QoL in knee OA; some studies report beneficial effects regarding improving general health (Sheth et al., 2014; Multani, 2005; Thorstensson et al., 2005; Dias CR et al., 2003) while other studies established that exercise is ineffective (Ravaud P et al., 2004; Lund et al., 2008). Due to the varying primary evidence it seemed important that a systematic review was conducted with the aim of summarising the evidence of relevant literature and providing more reliable and generalizable conclusions which could be used in clinical practice. Furthermore, identifying therapies that improve quality of life in patients with knee OA may lessen the clinical, economic and social burden of the disease (Farr II et al., 2013).
Methods, Data sources and Literature Search
The review was based on the Center for Reviews and Dissemination guide (CRD 2009) in order to remain focused on the research question and ensure consistency across all aspects of the review, and thereby reduce the risk of bias (Boland et al., 2014; Young and Solomon, 2009). A literature search of AMED, The COCHRANE LIBRARY, CINAHL, MEDLINE and PEDro was conducted in the middle of November 2014. To ensure a comprehensive search, Internet sources of Google Scholar were conducted to make sure that unpublished papers with registered databases were retrieved (CRD, 2009). While the review attempted to minimise publication bias (Greenhalgh et al., 2014), two non-English studies could not be included due to a lack of resources for translation.
Study selection
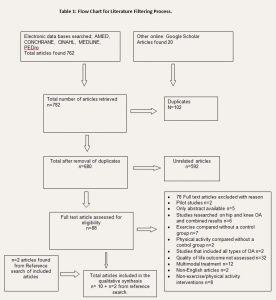
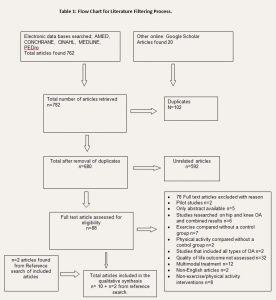
To ensure reliability of the decision process, a second reviewer was involved S.M. (CRD, 2009). To minimise selection bias selection criteria was clearly established and studies were included based on their eligibility. The criteria included; quantitative primary studies conducted in English, adult participates with clinically diagnosed knee OA, studies that investigated both knee and hip osteoarthritis, but reported the results separately for each area in order to extract data for knee OA and intervention that included exercise and or physical activity with a control group of alternative interventions. To ensure reliability of the results across studies (Fawcett 2007), only standardized scales were included; SF 36, Short Form SF-36, KOOS (Knee Injury and Osteoarthritis Outcome Score); Nottingham Health Profile (NHP); and other QoL scales. While the review aimed to include different types of quantitative studies other than RCTs in order to ensure a comprehensive review of available evidence, however, only RCTs and one quasi-experimental study met the requirement. In total 12 studies were reviewed as outlined in the flow chart below.
Quality Assessment
Quality assessment is important to ensure that included studies provided sufficient robustness for the results to be trustworthy and generalisable (Boland et al., 2014). Eleven RCTs and one quasi-experimental study met the inclusion criteria. The PEDro scale (available at www.pedro.org.au) was used to assess the methodological quality (Verhagen et al., 1998). Levels of scores were based on those outlined in a study by Abiebr (2011); study scoring below 4 was low quality, a score of 4-5 was moderate quality and 6-10 was high quality.
Table 1: Flow Chart for Literature Filtering Process.
Data extraction
Data extraction was undertaken by the author and a reviewer independently. Depending on evidence provided, results on QoL outcomes measures were extracted at two time points; post-treatment and follow-up results and were recorded as short-term (within three months) and long-term follow up (above three months) as shown in tables 2, 3a to 3d below. The reviewers discussed the findings and disagreement was resolved through dialogue.
To comprehensively assess QoL which is a influenced by variables such as age, physical and social functioning, emotional well-being, role activities, perceived health (Rejeski and Mihalko, 2001, Shumaker et al., 1990), results for each subscale were considered as they address these different aspects which ultimately determine QoL for an individual with a chronic disease such as knee OA.
Results
The literature search identified 782 studies; duplicates, unrelated studies were removed and remained with 88 potential studies for initial screening; 9 RCTs and 1 quasi-experimental study with 2 RCTs from reference search were included in the final review. 78 studies did not qualify, thus excluded.
Table 2: Characteristics of included studies

Key: Nottingham Health Profile questionnaire (NHP), verse (vs.), weeks (Wks.). Exercise (Ex), Quasi-Experimental study (Quasi-E)
3.1 Methodological Quality and risk of bias in the included studies
The quality of the studies is reported in table 2 above, the PEDro score ranged from 4 to 8 and the most common weakness were blinding (therapist, subjects and assessors) and intention to treat analysis. 10 high quality studies scores ranged from 6 to 8 and 2 moderate quality studies scored 4 and 5 respectively.
3.2. Study characteristics
To further understand the evidence, enhance transparency and prevent errors in interpretation, extracted data for study characteristics and results were tabulated as shown in table 3, 4a, 4b, 4c and 4d below. A total of 687 participants were included. The sample size ranged from n=31 (Aglamis et al 2008) to n=191 (O’Reilly et al., 1999).
3.3 Outcomes
The outcomes in tables 4a and 4b show statistical significance found by the authors of the different studies in p-values indicating either significant difference in support of the experimental group or no significant difference between the groups and confidence intervals (95%) with positive values in favour of the experiment group. They are reported according to short- or long-term follow-up for each outcome measure. The duration of interventions ranged from six weeks to six months respectively.
Studies were grouped into physical activity, exercise, aquatic exercise and exercise and physical activity when the interventions were combined, As per protocol, when two interventions were assessed with a control group, the results of one intervention in relation to the control group were reported, thus studies by Wang et al. (2011) and Lund et al. (2010) aquatic exercise were reported, and Evick and Sonel’s (2003) a walking programme instead of exercise was reported. This ensured that the review was inclusive for the type of exercise intervention.
Multicomponent strengthening exercise versus a non-intervention
The efficacy of multicomponent strengthening exercises in the management of OA was directly addressed in two high quality studies; Fransen et al., (2001) compared supervised group exercise supplemented with walking to a non-intervention group found significant improvement as reported on the SF 36 scale with the mental component score of CI 2.1 (0.8, 3.4) indicating a narrower confidence interval, and this was without the physical component score reaching statistically significant improvement. Similarly, Thorstensson et al. (2005) conducted a supervised multicomponent exercise complemented with a walking program and found on the SF 36 mental component score (p<0.04) in favour of the intervention.
Table 3a: Outcomes Results: SF 36 – mean percentage difference (95% confidence interval CI), P-value; Short term effects of exercise and physical activity < 3 months

Key: Combined Results for physical Mental and components (PC + MC), PEDro Score (PS), Exercise (Ex), Verses (vs), standardized response mean (SRM), Results not provided as a combined score
Table 3b: Outcomes Results: SF 36 – mean percentage difference (95% confidence interval CI), P-value; long term effects of exercise and physical activity < 3 months

Combined Results for physical Mental and components (PC + MC), PEDro Score (PS), Exercise (Ex), Verses (vs)
Table 3c: Outcomes for KOOS-QoL measure – mean percentage difference (95% confidence interval) and p=values where given

Combined Results for physical Mental and components (PC + MC), PEDro Score (PS), Exercise (Ex), Verses (vs)
Table 3d: Outcomes Results: Nottingham Health Profile questionnaire and p=values where given

Home based exercise and walking program versus non-intervention
Dias CR et al., (2003) evaluated the combined effects of walking with supervised progressive concentric-eccentric exercise to a non-intervention group. This moderate quality study reported statistically significant improvement in favour of exercise with functional capacity (p<0.000), physical role (p<0.0004) and general health (p<0.02) on the SF 36 scale. Similar findings were observed in a high-quality study by Aglamis et al., (2008) who reported significant improvement on most subscales of the SF 36 (p<0.001) with effects maintained at both 6 and 12 weeks’ follow-up after a supervised multicomponent functional exercise and walking programme.
Physical activity alone
Walking versus non-intervention
A moderate quality study by Evcik and Sonel (2002) compared the effects of a 3-month walking programme with a non-intervention group and found statistical and clinical improvement on all subscales of the Nottingham health profile (P<0.001) except for the social isolation dimension.
Exercise alone
Jorge et al. (2015) compared a supervised progressive strengthening programme with a no treatment group and found statistically significant improvement on SF 36 PCS; physical function and physical role (p-value 0.002, p-value 0.002) in favour of the exercise group. The MCS showed no improvement and the control group remained unchanged. While Salli et al. (2010) found that subjects receiving supervised concentric–eccentric exercise showed improvement on outcomes; SF36 PCS (P<0.001) at both 8 and 20 weeks follow-up while on the mental component of the scale, improvement above significant levels showed at 20 weeks follow-up.
Home based strength training
Three high quality studies; investigated the effectiveness of a home based strengthening exercise programme; Baker et al., (2001) compared progressive strengthening with a nutrition education group and evidenced statistically and clinically meaningful improvement in physical function, physical role, social function and mental health (p=0. 01, p<0.009, p<0.012 and p=0. 001) on the SF36 scale. However, the control group showed deterioration in QoL. Similarly, O’Reily et al (1999) conducted home based progressive isometric-isotonic exercises. While improvement was apparent in favour of the exercise, however the results were not significant as shown in table 4b. Doi et al. (2008) assessed home based quadriceps strengthening against non-steroidal anti-inflammatory drugs. Improvement was observed in both groups with positive results in favour of exercise (p<0.001) compared to NSAID (p, 0.023) however the significance difference appeared small. Some of this difference perhaps lies in the issue of motivation to undertake unsupervised exercise involving painful joints.
Aquatic Exercise Versus a non-intervention
High quality studies by Wang et al. (2011) and Lund et al. (2008) compared the effects of aquatic exercise involving strength training to non-intervention groups. Outcomes were reported using the KOOS, Wang et al. (2011) found statistical significant improvement on subscales; pain, symptoms, recreation, QoL (p<0.001). Other subscales showed less improvement and the control group remained unchanged. On the contrary, Lund et al. (2008) found no clinical benefits compared with the control group as shown in table 4c, however, the study reported significantly less adverse effects in the aquatic group.
3.5 Summary of evidence
Established on levels of evidence by Tulder et al. (2003) and the incorporated study quality to help interpret results (CRD 2009), findings of 8 high and 2 moderate quality studies provided strong evidence that exercise and physical activities are effective in improving QoL in knee OA. There is inconsistent evidence provided by two high quality studies on the efficacy of aquatic exercise. Overall, evidence from the majority of the studies demonstrated that the interventions could improve QoL with short term effects. Provided below is the table for the level of evidence.
Table 4: Level of evidence (Van Tulder et al., 2003).

4.0 Discussion
This systematic review summarised evidence from ten high and two moderate quality studies investigating the effectiveness of exercise and physical activity on QoL in knee OA. A number of potential studies were excluded mainly because they were a multimodal management. The review has provided strong evidence from eight high and two moderate quality studies that the interventions could be effective at improving QoL in knee OA. This evidence has established that regular, moderate levels of exercise do not aggravate symptoms in the majority of patients (Messier, 2010; McCarthy and Oldham, 1999). Further, a qualitative study by Wilcox et al. (2006) conducted on perceived exercise benefits, showed improvement, not only on pain and mobility, but also meaningful psychological benefits and enhanced QoL. This could be seen consistent with other studies that found the effects of exercise and physical activity improve self-efficacy and depression, which consequently resulted in improved QoL (Hartman et al., 2000; Penninx et al., (2002); Penninx et al., 2001; Singh et al., 2005; Beckwee et al., 2013)
The effects of strength training on the symptoms of knee OA are supported by wider literature, both of primary and systematic review studies. This is consistent with evidence from other studies that established the benefits of progressive strength training on symptoms in knee OA such as muscle atrophy and weakness which contribute to functional limitations and thereby restrict QoL (Jenkinson et al., 2009; Topp et al., 2002; Jan et al., 2008; Mikesky et al., 2005). Regular supervision as shown in Barker et al. (2001) and Evick and Sonel (2002) seemed to have positively influenced treatment outcome.
Activity is superior to all other treatments in the short term. This review observed that when exercise was compared with a non-intervention group, exercise results were significantly better. Whether this is most effectively performed on land or water remains unclear as included studies provided contradictory evidence. However when activity compared with other treatment groups (e.g. acupuncture), significant differences were small indicating some potential Hawthorne or placebo effects. However it could not be established if the interventions had long-term effects because of the limited number of studies that assessed long-term outcomes.
Overall, studies that included a supervised progressive multicomponent strengthening exercise, supplemented with a home exercise and walking programme found significant improvement in QoL (Jorge et al., 2015; Wang et al., 2011; Aglamis et al., 2008; Thorstensson et al., 2005; Dias CR et al., 2003. Baker et al., 2001; Fransen et al., 2001). This could suggest that physical activities not only provide relief of pain, but also those of psychological and general well-being as well as QoL (Aglamis et al., 2008; Dias CR et al 2003). Which activities are most effective remains uncertain however as Smith et al. (2014b) compared the effects of walking with cycling on QoL in OA knee and found that both groups improved with no statistically significant difference. This may indicate that exercise, although effective, may not be superior to other active interventions in terms of the impact on general wellbeing.
4.1 Strengths and limitations of this review
The review included primary studies of high quality and thoroughly reviewed the evidence provided. Publication bias could not be avoided as studies in other languages were removed and studies from less well-known databases may have been missed.
4.2 Strengths and limitations of included studies
The studies used standardised outcome measures to assess QoL but because they are not specific for measuring QoL in knee OA, they may not adequately assess the area. Based on the PEDro scale, quality studies from moderate to high were included on which evidence was drawn, however, common limitation in the studies was the lack of blinding of participants, therapists and assessors. Some studies had small sample size while some had drop-outs, but did not use intention to treat analysis, which could have impacted on the treatment effects (Joseph et al., 2014) and as a result, may not reflect a true clinical situation.
4.3 Implications: Clinical practice and Education
Clinically this suggests that exercise programmes designed to enhance QoL in knee OA patients ought to target specific impairments such as weakness, as presented in patients (Focht, 2012). This review observed a correlation between pain and QoL. A reduction in pain consequently resulted in improved QoL, thus, knowledge of the interplay of knee OA symptoms on QoL might help in understanding and management of patients. However biopsychosocial factors play a role and related co-morbidities may further complicate the situation (Chan and Wu 2012).
Treatment exercise plans, reinforced with a home exercise/walking programmes could help sustain the effects gained and consequently improve QoL. There is substantial evidence that physical activity has beneficial effects on QoL in knee OA, therefore, could be recommended for patients either as a facility or a home-based programme depending on the patient’s symptoms and preferences. In addition, included studies reported no serious adverse events indicating that moderate regular exercise and physical activity could be safe.
Future research may invest in developing a standardised outcome measure for QoL in knee OA and also developing a knee OA questionnaire assessing facilitators and barriers to exercise as increased understanding of the factors influencing exercise performance in people with OA could help physiotherapists and other health professionals support patients in initiating and maintaining an exercise routine and subsequently improve QoL post initial treatment.
Conclusion
Based on the available evidence, exercise and physical activity appear to be effective in improving knee OA symptoms and QoL. Land based exercise, well supervised home based exercises plus complemented with a walking programme provide significant improvement. Strength training exercises such as eccentric-concentric training provided better results. while exercises alone have short term effects, however, it could be established that these effects could be sustained when exercise and physical activity are incorporated into one’s lifestyle.
Acknowledgments
Dr Steven May and Mr Mahmoud Saad: Sheffield Hallam University – for guidance and support.
SM as the second article reviewer, many thanks.
Mambwe Mupeta MSc BSc (Hons) and Dr. Hazel Horobin Ed D
6.0 Reference list
ABIEBR, (2011). 1.6 DETERMINING LEVELS OF EVIDENCE. [Online]. Last accessed 21 October 2014 at: http://www.abiebr.com/set/1-introduction-and-methodology/16-determining-levels-evidence.
AGLAMIS B, TORAMAN NF, YAMAN H.The effect of a 12-week supervised multicomponent exercise program on knee OA in Turkish women. J Back Musculoskelet Rehabil2008;21:121–8.
AKERS, J., et al (2009). Systematic review. Centre for reviews and dissemination guidance for undertaking reviews in health care. York publishing service Ltd, USA.
AKINPELU, A., et al (2009). The prevalence of Symptomatic Knee Osteoarthritis in Nigeria. [Online] A Community Community-Based Study. 7, (3) 540-580.
ALKAN, B., ET AL 2014). Quality of life and self-reported disability in patients with knee osteoarthritis, [Online] Modern Rheumatology / The Japan Rheumatism Association, 24, (1), 166-171. Article from Medline EBSCO, Last accessed 25 October 2014 at: http://search.ebscohost.com/login.
ALTMAN, Douglas and BLAND Martine (2005). Statistics Notes: Treatment allocation by minimization. [Online] BMJ: British Medical Journal, 330 (7495), 843.
ALVES, J, and BASSITT, D (2013). Quality of life and functional capacity of elderly women with knee osteoarthritis. [Online] Einstein (São Paulo, Brazil), 11, (2), 209-215.
ANDERSON, C. (2010). Presenting and evaluating qualitative research.[Online]. American Journal of Pharmaceutical Education, 74 (8), 141.
BAKER, K.R., NELSON, M.E., FELSON, D.T., LAYNE, J.E., SARNO, R. and ROUBENOFF, R. (2001). The efficacy of home based progressive strength training in older adults with knee osteoarthritis: a randomized controlled trial. The Journal of rheumatology, 28(7), pp.1655-1665.
BARTOLUCCI, A. and HILLEGASS, W. (2010). Overview, Strength, limitations of systematic review and meta-Analysis. Evidence-Based Practice: Toward Optimizing Clinical Outcomes, 2, 1-8.
BATTERHAM, S.I., et al., (2011). Systematic review and meta-analysis comparing land and aquatic exercise for people with hip or knee arthritis on function, mobility and other health outcomes. BMC musculoskeletal disorders, 12(1), 123.
BECKWÉE, D., et al (2013). Osteoarthritis of the knee: Why does exercise work? A qualitative study of the literature. Ageing research reviews, 12(1), 226-236.
BENNELL K and HINMAN R (2005). Exercise as a treatment for osteoarthritis. Current Opinion in Rheumatology 2005; 17: 634–640
BENNELL, K., et al (2012). Management of osteoarthritis of the knee. [Online] BMJ (Clinical Research Ed.), 345, 4934.
BERNAD-PINEDA, M., et al (2014).Quality of life in patients with knee and hip osteoarthritis. [Online] Revista Española De Cirugía Ortopédica. 58, (5), 283-289.
BITTON, R. (2009). The Economic Burden Of Osteoarthritis. The American Journal Of Managed Care, 15(8), 230-5.
BOUTRON, I. et al., (2007). Reporting methods of blinding in randomized trials assessing nonpharmacological treatments. PLoS medicine, 4(2), 61.
BROSSEAU L, et al (2005). Efficacy of aerobic exercises for osteoarthritis (Part II): A meta-analysis. Physical Therapy Reviews, (9)125–145.
BOLAND A., CHERRY G. and DICKSON R. (2014). Doing a systematic review. A student’s guide. SAGE publication Ltd, London.
BROSSEAU L, et al (2005). Efficacy of aerobic exercises for osteoarthritis (Part II): A meta-analysis. Physical Therapy Reviews, (9)125–145.
CHACÓN, J.G. et al., (2004). Effect of knee osteoarthritis on the perception of quality of life in Venezuelan patients. Arthritis and rheumatism, 51(3) 377–82.
CHAIPINYO, Kanda and KAROONSUPCHAROEN, Orapin (2009). No difference between home-based strength training and home-based balance training on pain in patients with knee osteoarthritis: a randomized trial. [Online] The Australian Journal of Physiotherapy, 55, (1), 25-30.
CHAN, K. K. and CHAN, L. W. (2011). A qualitative study on patients with knee osteoarthritis to evaluate the influence of different pain patterns on patients’ quality of life and to find out patients’ interpretation and coping strategies for the disease. Rheumatology Reports, 3(1), 3.
CHAN, K. and WU, R. (2012). Symptoms, Signs and Quality of Life (QoL) in Osteoarthritis (OA). [Online] Principles of Osteoarthritis. Article from Medline EBSCO, last accessed 4 October 2014 at: http://search.ebscohost.com/login.
CLAUDE, B., et al (2007). Physical activity and health. Human Kinetics Publisher, Leeds.
COOK, C., et al (2007). Osteoarthritis and the impact on quality of life, health indicators. Rheumatology International, 27, (4), 315-321.
CENTRE FOR REVIEWS AND DISSEMINATION (2009). Evidence based guidelines and current practice for physiotherapy management of knee osteoarthritis Research articles Research articles. 745–56.
CROWTHER, David (2013). A clinician’s guide to systematic reviews. [Online] Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition, 28 (4), 459–62.
DIAS, C. R., DIAS, D.J.M. and RAMOS, L.R., 2003. Impact of an exercise and walking protocol on quality of life for elderly people with OA of the knee. Physiotherapy Research International, 8(3), pp.121-130. Last accessed at: http://doi.wiley.com/
DOI, T., AKAI, M., FUJINO, K., IWAYA, T., KUROSAWA, H., HAYASHI, K. and MARUI, E., (2008). Effect of home exercise of quadriceps on knee osteoarthritis compared with nonsteroidal antiinflammatory drugs: a randomized controlled trial. American Journal of Physical Medicine & Rehabilitation, 87(4), pp.258-269.
EGAN, B. and MENTES, J. (2010). Benefits of physical activity for knee osteoarthritis: a brief review. [Online] Journal of Gerontological Nursing, 36, (9), 9-14.
ESCALANTE, Y. et al., (2010). Physical exercise and reduction of pain in adults with lower limb osteoarthritis: a systematic review. Journal of back and musculoskeletal rehabilitation, 23(4)175–86.
ESSER, S. and BAILEY, A., (2011). Effects of exercise and physical activity on knee osteoarthritis. Current pain and headache reports, 15(6), 423–30.
EVCIK, D. and SONEL, B., (2002). Effectiveness of a home-based exercise therapy and walking program on osteoarthritis of the knee. Rheumatology international, 22(3), pp.103-106.
FARR II, J., et al (2013). Quality of life in patients with knee osteoarthritis: a commentary on nonsurgical and surgical treatments. [Online]The Open Orthopaedics Journal, 7, 619-623.
FARROKHI, S. and FITZGERALD, G.K., (2012). The Role of Physical Activity and Therapeutic Exercise in Development and Management of Knee Osteoarthritis. , 19(1), pp.27–36.
FOCHT BC, (2006). Effectiveness of exercise interventions in reducing pain symptoms among older adults with knee osteoarthritis: a review, (14)212–35.
FRANSEN, M., CROSBIE, J. and EDMONDS, J. (2001). Physical therapy is effective for patients with osteoarthritis of the knee: a randomized controlled clinical trial. The Journal of rheumatology, 28(1), pp.156-164.
FRANSEN M., et al (2002).Therapeutic exercise for people with osteoarthritis of the hip or knee. A systematic review. J Rheumatol, (29)1737-45.
FRANSEN, M. et al., (2011). The epidemiology of osteoarthritis in Asia. [Online] International journal of rheumatic diseases, 14 (2)113–21
FRANSEN, M. & MCCONNELL, S., (2008). Exercise for osteoarthritis of the knee. Cochrane Database Syst Rev, (4). Accessed October 25, 2014.
JENKINSON CM. et al. (2009). Effects of dietary intervention and quadriceps strengthening exercises on pain and function in overweight people with knee pain: randomised controlled trial. BMJ, 339(3)170.
JORGE, R.T.B., SOUZA, M.C.D., CHIARI, A., JONES, A., FERNANDES, A.D.R.C., JÚNIOR, I.L. and NATOUR, J., (2015). Progressive resistance exercise in women with osteoarthritis of the knee: a randomized controlled trial. Clinical rehabilitation, 29(3), pp.234-243.
JOSEPH, R. et al., (2015). A systematic review finds variable use of the intention-to-treat principle in musculoskeletal randomized controlled trials with missing data. Journal of clinical epidemiology, 68(1), 15–24.
HEARN, J. et al., (1999). Issues in research: Systematic reviews. Palliative Medicine, 13(1), 75–80.
HEIDARI, B., (2011). Knee osteoarthritis prevalence, risk factors, pathogenesis and features: Part I, Caspian Journal Of Internal Medicine, 2, (2), 205-212.
HURLEY M.V. (2003). Muscle dysfunction and effective rehabilitation of knee osteoarthritis outcomes: What we need to find out. Arthritis Rheum.
GLASGOW, R. E., et al (2003). Why don’t we see more translation of health promotion research to practice? Rethinking the efficacy-to-effectiveness transition. American Journal of Public Health, 93(8), 1261-1267.
GREENHALGH, T. (2014). How to read a paper: the basis of evidence based medicine. 5th ed, Chichester, Wiley.
GUPTA, S. K. (2011). Intention-to-treat concept: A review. Perspectives in clinical research, 2(3), 109.
HIGGINS, Julia and GREEN, Sally (2008). Cochrane handbook for systematic reviews of interventions. Chichester: Wiley-Blackwell.
HOPMAN, W., et al (2009). Associations between chronic disease, age and physical and mental health status. [Online] Chronic Disease in Canada, 29 (2), 108–117.
LIBERATI, A. et al., (2009). The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. [Online] Medicine, 6 (7), 100.
LUND, H., WEILE, U., CHRISTENSEN, R., ROSTOCK, B., DOWNEY, A., BARTELS, E.M., DANNESKIOLD-SAMSØE, B. and BLIDDAL, H., (2008). A randomized controlled trial of aquatic and land-based exercise in patients with knee osteoarthritis. Journal of rehabilitation medicine, 40(2), pp.137-144.
JAN MH. et al (2008). Investigation of clinical effects of high and low-resistance training for patients with knee osteoarthritis: a randomized controlled trial, 88(4):427–36. 57.
JOHNSON, V., and HUNTER, D. (2014).The epidemiology of osteoarthritis. [Online] Best Practice & Research. Clinical Rheumatology, 28, (1), 5-15.
KHAN, K and KUNZ, R, (2011). Systematic reviews. To support evidence based medicine. 2nd edition. Hodder & Stoughton Ltd. UK.
KAO, M., et al (2012).The effectiveness of a self-management program on quality of life for knee osteoarthritis (OA) patients, [Online] Archives Of Gerontology And Geriatrics, 54, 2, pp. 317-324.
LANGE, A.K., et al (2008). Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis and rheumatism, 59(10), 1488–94.
LARMER, P., et al (2014). Systematic review of guidelines for the physical management of osteoarthritis, [Online] Archives of Physical Medicine and Rehabilitation, 95, 2, pp. 375-389.
LAVER-FAWCETT, A. (2007). Principles of assessment and outcome measurement for occupational therapists and physiotherapists: theory, skills and application. John Wiley & Sons Ltd, London.
LITTLEWOOD C. and MAY, S. (2013). Understanding Physiotherapy Research. Newcastle, Cambridge Scholars Publishing.
LITWIC, A., et al (2013). Epidemiology and burden of osteoarthritis. [Online] British Medical Bulletin, 105, 185-199.
MAHER, C. G., et al (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical therapy, 83(8), 713-721.
MAJANI, G., et al (2005). Subjective impact of osteoarthritis flare-ups on patients’ quality of life. Health and quality of life outcomes, 3, .14.
MANNINEN, P. et al., (2001). Physical exercise and risk of severe knee osteoarthritis requiring arthroplasty. 432–437.
MCCARTHY CJ and OLDHAM JA (1999). The effectiveness of exercise in the treatment of osteoarthritic knees: a critical review. Phys TherRev 1999; 4:241–50
MESSIER, S. P. (2010). Diet and exercise for obese adults with knee osteoarthritis. Clinics in geriatric medicine, 26(3), 461.
MICHAEL, J., et al (2010). The epidemiology, aetiology, diagnosis, and treatment of osteoarthritis of the knee. [Online] Deutsches Aerzteblatt International. 107, (16), 294.
MIKESKY AE., et al (2006). Effects of strength training on the incidence and progression of knee osteoarthritis. Arthritis Care Res. 55(5):690–9.59.
MOHER, D., et al (2012). CONSORT 2010 explanation and elaboration: Updated guidelines for reporting parallel group randomized trials. [Online] International Journal of Surgery, 10 (1), 28-55.
MULTANI NK (2005). The changing role of Physiotherapists in the management of osteoarthritis knee, “Physiotherapy”. The Journal of The Indian Association of Physiotherapist,(1)15-20.
NAJAFABADI, M.T et al., (2014). Asian Journal of Multidisciplinary Studies Available online at www.ajms.co.in Comparison of isometric and Pilates exercises on Knee pain and quality of life in women with Knee Osteoarthritis. , 2(3), pp.109–112.
NGUYEN, U., et al (2011). Increasing prevalence of knee pain and symptomatic knee osteoarthritis. [Online] Annals of Internal Medicine, 155 (11) 725-732,
NIGHTINGALE, A. (2009). A guide to systematic literature reviews. Surgery (oxford), 27 (9), 381-384.
O’REILLY, S.C., MUIR, K.R. and DOHERTY, M., (1999). Effectiveness of home exercise on pain and disability from osteoarthritis of the knee: a randomised controlled trial. Annals of the Rheumatic Diseases, 58(1), pp.15-19.
PAGE, M., et al (2014). Bias due to selective inclusion and reporting of outcomes and analyses in systematic reviews of randomized trials of healthcare interventions, The Cochrane Database Of Systematic Reviews, 10, 35.
PELLAND, L. et al., (2004). Efficacy of strengthening exercises for osteoarthritis. Physical Therapy Reviews 9: 77–108
PENNINX B.J., et al (2001). Physical Exercise and the Prevention Disability in Activities of Daily Living in Older Persons With Osteoarthritis, (161)2309-16.
PENNINX, B.W., et al (2002). Exercise and depressive symptoms: a comparison of aerobic and resistance exercise effects on emotional and physical function in older persons with high and low depressive symptomatology. Journals of Gerontology, 57, 124–132.
PETURSDOTTIR, U., et al (2010). Facilitators and barriers to exercising among people with osteoarthritis: a phenomenological study. Physical therapy, 90(7), 1014–25.
PHILLIPS, S., et al (2013). Physical activity and quality of life in older adults: an 18-month panel analysis. [Online] Quality Of Life Research: An International Journal Of Quality Of Life Aspects Of Treatment, Care And Rehabilitation, 22, (7), 1647-1654,
PIETROSIMONE, B., et al (2014). Association between quadriceps strength and self-reported physical activity in people with knee osteoarthritis, [Online] International Journal of Sports Physical Therapy, 9, (3), 320-328.
REJESKI, W. J., AND MIHALKO, S. L. (2001). Physical activity and quality of life in older adults. The Journals of Gerontology Series A: Biological Sciences and Medical Sciences, 56(2), 23-35.
RIDDLE, D.L., et al (2011). Psychological health impact on 2-year changes in pain and function in persons with knee pain: data from the osteoarthritis initiative. Osteoarthritis and cartilage/OARS. Osteoarthritis Research Society, 19, 1095–1101.
ROTONDI, M. and DONNER, A., (2012). Sample size estimation in cluster randomized trials: An evidence-based perspective. Computational Statistics & Data Analysis, 56(5), 1174–1187.
SACKETT, D. L. and WENNBERG, J. E. (1997). Choosing the best research design for each question. BMJ, 315 (7123), 1636.
SALLIi, A., SAHIN, N., BASKENT, A. and UGURLU, H., (2010). The effect of two exercise programs on various functional outcome measures in patients with osteoarthritis of the knee: A randomized controlled clinical trial. Isokinetics and Exercise Science, 18(4), pp.201-209.
SHERRINGTON, C., et al (2003). Reliability of the PEDro scale for rating quality of randomized controlled trials. Physical therapy, 83(8), 713-721.
SHUMAKER SA, et al (1990). Psychological tests and scales. Quality of Life Assessments in Clinical Trials. New York: Raven Press.
SILVA, L.E. et al., (2008). Hydrotherapy versus conventional land-based exercise for the management of patients with osteoarthritis of the knee: a randomized clinical trial. Physical therapy, 88(1), 12–21.
SINGH, N.A., et al (2005). A randomized controlled trial of high versus low intensity weight training versus general practitioner care for clinical depression in older adults. The Journals of Gerontology, (60), 768–776.
SMINK, A., et al (2011).”Beating osteoarthritis”: development of a stepped care strategy to optimize utilization and timing of non-surgical treatment modalities for patients with hip or knee osteoarthritis, [Online] Clinical Rheumatology, 30, (12), 1623-1629.
SMITH, T., et al (2014a). A systematic review to determine the optimal type and dosage of land-based exercises for treating knee osteoarthritis.[Online] Physical Therapy Reviews, 19 (2),105-113.
SMITH, T., et al (2014b). Living with osteoarthritis: a systematic review and meta-ethnography, Scandinavian Journal of Rheumatology, 1-12.
TALBOT LA., et al (2003). A home-based pedometer-driven walking program to increase physical activity in older adults with osteoarthritis of the knee: A preliminary study. J Am Geriatric, 51(3)387–392.
THOMAS K, et al (2002). Home based exercise programme for knee pain and knee osteoarthritis: randomised controlled trial. BMJ, (325)752–5.
THORSTENSSON, C.A., ROOS, E.M., PETERSSON, I.F. and EKDAHL, C., (2005). Six-week high-intensity exercise program for middle-aged patients with knee osteoarthritis: a randomized controlled trial [ISRCTN20244858]. BMC Musculoskeletal Disorders, 6(1), p.27.
TOPP R., et al (2002). The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Arch Phys Med Rehab, 83:1187–95.
VEENHOF, C., et al (2012). Factors associated with physical activity in patients with osteoarthritis of the hip or knee: a systematic review, Osteoarthritis and Cartilage / OARS, Osteoarthritis Research Society, 20, (1), 6-12.
VENNU, V., and BINDAWAS, S. (2014). Relationship between falls, knee osteoarthritis, and health-related quality of life: data from the Osteoarthritis Initiative study, Clinical Interventions in Aging, 9, 793-800.
YILMAZ, H., et al (2013). Effectiveness of home exercise program in patients with knee osteoarthritis. European Journal of General Medicine, 10, (2), 102-107.
YOUNG, Jane and SOLOMON, Michael (2009). How to critically appraise an article. Nature Clinical Practice. Gastroenterology & Hepatology, 6 (2), 82-91.
WANG, T.J., LEE, S.C., LIANG, S.Y., TUNG, H.H., WU, S.F.V. and LIN, Y.P., (2011). Comparing the efficacy of aquatic exercises and land‐based exercises for patients with knee osteoarthritis. Journal of clinical nursing, 20(17‐18), pp.2609-2622.
WILCOX, S. et al., (2006). Perceived exercise barriers, enablers, and benefits among exercising and nonexercising adults with arthritis: results from a qualitative study. Arthritis and rheumatism, 55(4), 616–27.
WOOLF, A.D. and PFLEGER, B., (2010). Burden of major musculoskeletal conditions. 81(03).
WORLD HEALTH ORGANISATION (2010). Definition of physical activities. [Online] last accessed 25 October 2014 at: http://www.who.int/topics/physical_activity/en/
ZHANG, C., et al. (2008). OARSI recommendations for the management of hip and knee osteoarthritis, Part II: OARSI evidence-based, expert consensus guidelines Osteoarthritis and Cartilage / OARS, Osteoarthritis Research Society, 16 (12), 1585-1589.
ZHANG, Y. and JORDAN, J. (2010). Epidemiology of osteoarthritis. Rheumatic Diseases Clinics of North America, 34 (3) 515-529.
ZAZA, S., et al (2000). Data collection instrument and procedure for systematic reviews in the Guide to Community Preventive Services. Task Force on Community Preventive Services, [Online] American Journal of Preventive Medicine, 18, (1) 44-74.
 The hospital Trust has gained confidence in the merits of involving student volunteers and more projects and new collaborations have since been generated. Students add value to bespoke projects that otherwise might not have taken place. Students have referred to their volunteering experiences at employment interviews and reported favourable responses.
The hospital Trust has gained confidence in the merits of involving student volunteers and more projects and new collaborations have since been generated. Students add value to bespoke projects that otherwise might not have taken place. Students have referred to their volunteering experiences at employment interviews and reported favourable responses.