Introduction
There are currently unprecedented levels of demand on urgent and emergency care throughout the UK (University of Sheffield Medical Care Research Unit 2010; Agarwal et al, 2011; NHS England 2013), with ED attendances and ambulance call outs increasing consistently every year (Nelson 2011; Newton et al, 2013). Accident and Emergency (A&E) departments are regularly missing the four-hour waiting target (NHS England 2013; BBC 2015) and there is national concern over the National Health Service’s (NHS) ability to cope with the increasing pressure (Press Association 2013; Cooper 2015).
With potentially 15% of the UK population utilising urgent and emergency care services at any one time, many accessing multiple services (Knowles, O’Cathain & Nicholl 2010), it is important to ensure appropriate use of frameworks in order to avoid any one service becoming over-burdened.Congested A&E departments have a direct and significant impact on ambulance service performance (National Audit Office 2011; NHS England 2013; Mundasad 2014), and whilst the link between ambulance and ED services should be fundamentally evident (National Audit Office 2011; Patton & Thakore 2012), often the two services are treated as isolated and even opposing entities. One example of this is the proposal of ‘forced handovers’ by ambulance crew in certain trusts (Johnston 2015; Local Ambulance Trust 2015).
The Bradley Report (Department of Health 2005) marked a fundamental recognition that ambulance services could not only reduce the amount of people admitted to A&E, but that this reduction could have a significant impact on emergency care and wider NHS services. The aim of this literature review was to establish how ambulance services can help reduce current demand on wider urgent care services and A&E departments in particular, through a greater awareness of inappropriate patient use, what causes it and how alternative care pathways can be utilised in order to reduce it. In doing so, this paper also aims to demonstrate the fundamental connection between ED and ambulance services, and how their performance is mutually dependant on one another.
Two semi-structured literature searches were conducted of CINAHL, PubMed, AMED, Cochrane Library databases and the Journal of Paramedic Practice; one exploring inappropriate use of services and one exploring prehospital admission avoidance. Twenty-seven articles were included for review and four broad themes were identified; Definition of Terms, Patient Factors, Access to Healthcare and Healthcare Frameworks.
A high number of diverse and complex contributors to inappropriate emergency department (ED) attendance and ambulance use were identified. Whilst some patient factors contributed towards this issue, problems with wider healthcare frameworks and organisational behaviours were significantly more abundant in reviewed literature. Fragmentation of services may be creating barriers to alternative care services to both patients and clinicians attempting to make referrals. Strategies to improve appropriate use of healthcare should focus on enhancing the way in which services work together.
Methodology
A systematic search was performed using an adapted methodology from Moher et al (2009). CINAHL, PubMed and Cochrane Library databases were searched for key phrases in the title or abstract. A secondary search was conducted of the same databases using phrases including ‘Ambulance’, ‘Admission Avoidance’ and ‘Pathway’.
Additional keywords derived from iterative searches were added to search terms until appropriate saturation of results had been achieved. Boolean operators ‘AND’ and ‘OR’ were utilised to broaden and narrow results accordingly (Machi & McEvoy 2009).
Articles were critically analysed using a tabular matrix adapted from LoBiondo-Wood and Haber (2013). Key issues from each article where then extracted to create a thematic index (Thomas, Harden & Newman 2012).
Research conducted outside of the UK was excluded due to the internationally unique framework of the National Health Service. The exception to this was material considered in systematic reviews, where articles were included as long as they were written in the UK. Articles which focused solely on self-presentation at the ED, or which did not make any explicit differentiation between routes of attendance were also excluded. Articles published before 2010 was excluded due to changes in GP out-of-hours (OOH) services.
Material focusing upon paediatrics or specific medical complaints was excluded, with the exception of falls, and frequent users. All levels of evidence were included (National Institute for Health and Care Excellence 2006), with the exception of narrative expert opinion due to the limited quality of this evidence (GRADE Working Group 2004).
Definition of Terms
Of all reviewed material, only ten articles (Endacott et al, 2010; Agarwal et al, 2011; Jones 2011; May 2011; Patton and Thakore 2012; Booker, Simmonds and Purdy 2013; Newton et al, 2013; O’Cathain et al, 2013; O’Hara et al, 2014; Atenstaedt et al, 2014) explained how they classified inappropriate use, and of these, only a very few demonstrated significant effort to objectify definitions. Articles that did rigorously establish objectivity showed variation in their presented views. The University of Sheffield Medical Care Research Unit (2010) highlights significant inconsistency in defining appropriateness throughout healthcare research. Furthermore, Jones (2011) and Booker, Simmonds and Purdy (2013) argue that appropriateness is almost exclusively defined retrospectively by healthcare staff. This demonstrates the complexity of this particular area, and may explain conflicting views of appropriateness between ED and prehospital clinicians (Newton et al, 2011; Patton & Thakore 2012). However, whilst there exists significant challenges in objectively defining inappropriate use, clarification on what this looks like is crucial in aiding clinicians to identify and reduce it in real terms. Further research in this area would be beneficial in providing clearer guidelines for prehospital clinicians when dealing with potentially inappropriate use.
Patient Factors
A significant proportion of extracted themes related to subjective factors influencing individual patient behaviour. These could be categorised into four main sub-themes; Perception of Illness, Interpersonal Factors, Patient Demographics and Socioeconomic Factors.
Perception of Illness
Booker, Simmonds & Purdy (2013) found symptom and decision-making anxiety to be the superordinate theme of their research, often resulting in risk-averse decisions to summon the most immediate form of assistance. Whilst recognised methods were used to conduct thematic analysis, questionnaire content was derived from a previous pilot, rather than established evidence, resulting in potential content bias (Pannucci, & Wilkins 2010). However, this research was externally peer-reviewed, and several further articles provide consensus on this finding (Agarwal et al, 2011; University of Sheffield Medical Care Research Unit 2010; Edwards et al, 2014).
Conversely however, a literature review by Sheffield University (University of Sheffield Medical Care Research Unit 2010) highlights that misconceptions of symptoms can potentially cause inappropriate delay or refrain from contacting emergency services. Whilst the aforementioned makes no analysis of the ratio between inappropriate contact and non-contact, Kirkby and Roberts (2011) suggest that the majority of inappropriate classification occurs when no ambulance is required.
Patient education was highlighted as pivotal in several articles (Atenstaedt et al, 2014; Patton & Thakore 2012; Jones 2011; Kirkby & Roberts 2011). Atenstaedt et al (2014) demonstrates the effectiveness of targeted campaigns in improving patient knowledge and reducing inappropriate attendance, however provides no cost-analysis of these strategies. Perhaps a cost-effective opportunity exists for the ambulance service to deliver this type of patient education to inappropriate users. The ambulance service has previously demonstrated high levels of success in bringing health campaigns to public awareness (Association of Ambulance Chief Executives 2011). This is demonstrated by the recent stroke awareness campaign by the South East Coast Ambulance Service (South East Coast Ambulance Service 2015).
Interpersonal Factors
Similarly three articles considered interpersonal factors such as relatives and carers in the decision-making process. Booker, Simmonds & Purdy (2013) found interpersonal factors often reduced tolerance for medical risk. They found that informal carers often experienced feelings of responsibility and helplessness, prompting them to take the least risky course of action. In addition, risk-minimising behaviour was noted in patients themselves, who often felt pressured by what friends and family might think, regardless of their actual presence. Whilst a single site limits this research’s external validity (Steckler & McLeroy 2007), verbatim transcripts noted this as a reoccurring theme in interviews. The Association of Ambulance Chief Executives (2011) outlines similar risk-averse behaviour from staff in care homes, however primarily driven by misconceptions of organisational responsibility.
The Keogh Review (NHS England 2013) suggests that self-care is a crucial influencer of service demand. In many cases this is dependant on patient and carer confidence managing minor ailments and long-term conditions.
Interpersonal factors can significantly influence subsequent use of ambulance services, and therefore should be considered by the prehospital clinician when attending an incident. It is also important for clinicians to recognise how interpersonal factors and support networks can influence a patient’s ability to self-manage, as this is pivotal information when making referral or non-conveyance decisions. In addition, clinicians should be aware interpersonal pressures when assessing patient wishes and when making best interest decisions.
Patient Demographics
The Keogh Review (NHS England 2013) identifies that the patient demographics most likely to benefit from alternative healthcare support are those least likely to be aware of it, prompting increased inappropriate dependence on urgent services. Several articles studied the effect of patient demographics on healthcare usage. Whilst Kirby and Roberts (2011) found no statistically significant factors in their research, Dent, Hunt and Webster (2010) found that frequent ED attenders were more likely to be male, with a mean age of 49. In a systematic review, Scott et al (2013) finds several concurring articles identifying frequent users as predominantly male. Despite some potential bias introduced from a single initial reviewer, established methodology and quality analysis is employed.
Edwards et al (2014) and Smith and McNally (2014) both agree that elderly demographics can make up a significant portion of inappropriate and frequent users. However, Scott et al (2013) found highly mixed evidence in regards to patient age, and only one limited study suggesting that frequent use increased with age.
Reviewed literature demonstrates mixed evidence in relation to patient demographics, and caution should be taken by the prehospital clinician in stereotyping frequent or inappropriate users of healthcare (Donohoe & Blaber 2008). The majority of evidence suggests that inappropriate users are heterogeneous, presenting for a variety of health and social reasons (Edwards et al, 2014; Scott et al, 2013).
Socioeconomic Factors
In a quantitative ecological study, O’Cathain et al (2013) found that areas of social deprivation, and urban areas had significantly higher numbers of avoidable emergency admissions. Whilst many confounding variables were not considered in this research, including distance to hospital, these factors were statistically calculated as significant, with a combined predictor of 75% in admission avoidance variation. In addition, many articles support this finding (Agarwal et al, 2011; Association of Ambulance Chief Executives 2011; Scott et al, 2013; Edwards et al, 2014; Smith & McNally 2014).
Conversely to O’Cathain, O’Hara et al (2015) suggested through qualitative research that rural areas had limited access to alternative pathways, and were more likely to see increased inappropriate ambulance transport. However, this research was limited by a small sample size at risk of self-selected participant bias (Lavrakas 2008). This furthermore contradicts evidence from the National Audit Office (2011) highlighting increased ‘see and treat’ rates in rural areas.
Whilst there exists conflicting views regarding geographical influence on appropriate healthcare use, there is an overwhelming consensus of evidence suggesting social deprivation contributes towards inappropriate and frequent use of urgent services. Healthcare campaigns have demonstrated success when socioeconomically targeted (Atenstaedt et al, 2014), and strategies by ambulance services to manage inappropriate use appear well advised to be initially targeted at economically deprived areas.
Access to Community Care Services
Several articles discuss patient access to community services as an influencing factor of avoidable ED attendance and inappropriate ambulance use. The Keogh Review (NHS England 2013) highlights significant variation in GP service satisfaction levels nationally, with systemic fragmentation of community services causing further access issues. This is supported by Agarwal et al (2011), which found GP access issues to be a consistently reoccurring theme in patients attending the ED inappropriately. In similar semi-structured interviews, Booker, Simmonds and Purdy (2013) also found that previous experience accessing community services and perceived limitation of GP capabilities heavily influenced patients’ decision to access ambulance services with primary care issues. This might explain why in highly rigorous, mixed-method action research, Endacott et al (2010) found that inappropriate ED attendances increased dramatically during OOH periods. If barriers to community care increase rates of inappropriate ambulance and ED usage, this has significant implications for ambulance services in analysing patterns of demand and managing response levels geographically and at different time periods (NHS Office of Strategic Health Authorities 2008). Evidence also suggests ‘post code’ variation in access to GP services (Raleigh & Frosini 2012; NHS England 2013), and further research into this area is warranted.
O’Cathain et al (2013) found that patients’ perception of good access to GP services was initially linked to lower ED attendance rates at primary stages of analysis, however when considering further variables such as overall ED and ambulance demand, actually contributed to higher attendance rates through GP referral. Indeed, Turner et al (2013) outlines the potential for supplier-induced demand, particularly in the area of alternative community services such as NHS 111. The Keogh Review (NHS England 2013) supports this notion, and furthermore highlights that GP consultations have also been increasing, despite expansion of alternative services. Therefore the issue may be more related to general demand rather than patient access. This is supported by Edwards et al (2014), which found that frequent use of emergency services was linked to equivalent frequent use of other community services.
However, as Patton and Thakore (2012) found GP referrals via the ED were associated with lower levels of inappropriateness, it is still reasonable to suggest that better access to GP services could improve avoidable ED admission rates. This is supported by Jones (2011), which, despite limitations in external validity (Steckler & McLeroy 2007), saw on-site GPs contribute to a reduction in avoidable admissions and improved waiting times at one district hospital ED. Paramedic Practitioners are now working more closely in supporting community GP services (Association of Ambulance Chief Executives 2011), and therefore perhaps this should be an important focus by ambulance trusts in managing overall demand.
Convenience of Emergency Services
Inversely, ease of access to ambulance and emergency department services was also a reoccurring contributor to inappropriate use of these channels. Patton and Thakore (2012) surmise that the convenience of an ED providing 24-hour investigations without appointment must significantly influence patient behaviour, however this was not explicitly analysed in their research. Smith and McNally (2014) propose a similar rationale for frequent users of urgent and emergency care services, and furthermore speculate a similarity in the behaviour of ED and ambulance users; a view supported by Edwards et al (2014). The notion of access simplicity is also supported by Knowles, O’Cathain and Nicholl (2010), who found that multiple referral pathways were linked with lower levels of satisfaction in the majority of patients. Through random quota telephone surveys, this paper also found high levels of satisfaction with Ambulance and ED services in particular, despite low levels of satisfaction with GP OOH and NHS Direct services. Indeed, the Keogh Review confirms that patient experience of ‘999’ emergency services is consistently positive; “overwhelmingly” so for patients with non-urgent conditions (NHS England 2013, 26).
Agarwal et al (2011) found confusion over alternative pathways to be a main contributor to patients accessing urgent services inappropriately. Participants in this research cited familiarity of services, and perception of efficiency over GP services as important influencers on the decision to attend the ED. Similarly, Booker, Simmonds & Purdy (2013) found users quoted previous positive experience and convenience of access to be primary contributors in their decision to access urgent care.
All articles appeared to demonstrate generally high levels of satisfaction amongst patients utilising ambulance and ED services, putting these services in the predicament of generating increased demand through positive performance. This represents a significant dilemma for the NHS, as these channels are by far the most expensive routes for patients to access health services (NHS England 2013). In addition, recent declining patient satisfaction levels for ED services demonstrate the consequences of demand surpassing a service’s capacity (NHS England 2013).
However, if adequately resourced, this could be viewed as an opportunity for the NHS to give more robust signposting and referral powers to a service with which patients are already confident using (National Audit Office 2011; Booker, Simmonds & Purdy 2013; Smith & McNally 2014). Patton and Thakore (2012) find that ambulance admission avoidance could reduce demand on ED services by 11%; a view supported by established literature (Department of Health 2005; The Association of Ambulance Chief Executives 2011). In addition to improving the overall profile of the ambulance service within the NHS, the National Audit Office (2011) estimates that this would be a significantly more cost-effective response model if configured appropriately.
Healthcare Frameworks
The Francis enquiry (2013) demonstrates how an organisational culture, and clinical behaviours within that culture, can have a significant impact on the quality of healthcare delivered to patients. A large majority of articles considered organisational and clinician factors in relation to inappropriate and frequent use of emergency care. Extracted themes could be broadly categorised into four subheadings; Triage and Clinical Decision-Making, Multidisciplinary Collaboration, Specialised Roles and Service Management.
Triage and Clinical Decision-Making
Sensitive triage and risk-averse behaviour are an integral part of NHS culture (NHS England 2015), and whilst risk management is an important consideration for any healthcare system (Turner et al, 2013; O’Hara et al, 2014), it can also contribute towards inappropriate use of emergency channels.
Patton and Thakore (2012) demonstrate the potential impact of oversensitive triage from ambulance staff. They found that a third of ED attendances were transported via ambulance, and of these admissions, 30% were deemed inappropriate. Whilst a potential bias exists with the duty consultant subjectively assessing appropriateness, reviewers did rotate throughout the study, and rigorous assessment was made using both the ED notes and Patient Report Form (PRF). Further articles support the suggestion of inappropriate ED referral through risk-averse or unsuitable ambulance triage (Newton et al, 2013; University of Sheffield Medical Care Research Unit 2010; O’Hara et al, 2014). However, Newton et al (2013) and O’Hara et al (2014) highlight the complexity of prehospital decision-making, particularly with low-acuity incidents.
A recent qualitative exploration of current treat and refer guidelines (Colver, Abhyankar & Niven 2015) highlights variation in prehospital use, and suggests further education and support for clinicians. In addition, Newton et al (2013) demonstrates the moderate success of prehospital pathway finders adapted from the Manchester Triage System. However, whilst providing clinicians with support tools may improve confidence, it may be argued that such tools do not address the issue of clinician education, and furthermore may be inappropriate for clinically and socially complex situations.
Oversensitive triage was also outlined as a primary contributor to increased ambulance workload by telephone services such as NHS ‘111’ (Turner et al, 2013). The issue of over-triage through telecommunications is furthermore supported in several articles (University of Sheffield Medical Care Research Unit 2010; Knowles, O’Cathain & Nicholl 2010; NHS England 2013). In this respect, the potential of a ‘snowballing’ effect of systemic over-triage through multiple services can be observed (Department of Health and Ageing 2007).
A proposed solution to this may be the implementation of secondary triage systems (Eastwood et al, 2014) in order to decrease sensitivity whilst maintaining risk management. However there exists little evidence on the most appropriate structure or benefits of this within a prehospital framework, and further research is warranted.
Multidisciplinary Collaboration
As previously discussed there are some perceived and tangible patient access issues to community care services (Booker, Simmonds & Purdy 2013), and this is also reflected in prehospital referral pathways (O’Hara et al, 2014).
The National Audit Office (2011) highlights the importance of multi-service collaboration in reducing overall demand, and the knock on effect when one service becomes congested. This is supported by further articles (Booker, Simmonds & Purdy 2013; NHS England 2013), which suggest that fragmentation of services is a heavy contributor to inappropriate use. Indeed Edwards et al (2014) and Smith and McNally (2014) both concur that collaborative multi-level interventions are most effective in tackling frequent and inappropriate use, whilst Booker, Simmonds and Purdy (2013) call for closer collaboration between primary care and ambulance services.
In a mixed-method qualitative study, O’Hara et al (2014) identifies the lack of available care alternatives as a key contributor to inappropriate ED attendance via ambulance. Whilst this was a relatively small study, this theme reoccurred consistently throughout three individual trusts, suggesting a high level of reliability (May 2011). However, the National Audit Office (2011) highlights a paucity of ambulance trusts adequately collating directories of alternative services, suggesting that the underlying issue may be prehospital awareness, rather than availability.
Specialised Roles
In a literature review by Coates (2013), Emergency Care Practitioners (ECP) were found to significantly reduce the number of patients conveyed to hospital, with estimates of approximately £20k in annual ED cost reduction per ECP. This is furthermore supported by Mason et al (2010), which found that ECPs increased admission avoidance rates, and were most effective in a mobile setting.
However Coates (2013) rightly questions the difference between avoided admission and avoided ED attendance, highlighting a paucity of studies differentiating between the two. Since a significant cost difference is applicable, further research in this area should be considered.
Reviewed material demonstrates that specialised roles have a significant benefit on admission avoidance, concurring with established literature (National Audit Office 2011; Association of Ambulance Chief Executives 2011). However, there is still variability in the deployment of these roles (NHS England 2013), and whilst there remains such a heavy prehospital focus on targeted response times over clinical outcomes (National Audit Office 2011), it may be argued that specialised prehospital roles cannot be utilised to their fullest potential.
Service Management
O’Hara et al (2014) highlighted several organisational factors which influenced clinical decisions to transport patients to the ED when alternative care may have been more appropriate. These included availability of diagnostic equipment, availability of remote support and appropriate initial staff deployment. Clinicians also felt that lack of vehicles and resources increased the pressure to reduce on-scene times, prompting them to avoid time-consuming referral pathways. Endacott et al (2010) also identifies inconsistencies in ED management of inappropriate attenders. Despite having debatable direct impact on ambulance services, this demonstrates the difficulty of managing inappropriate use in a controlled environment, and suggests greater management complexities in the prehospital setting. Indeed, Edwards et al (2014) outlines the challenges of individual case management for frequent users.
In addition, the University of Sheffield Medical Care Research Unit (2010) outlines the difficulty of service management across boundaries, and how tensions between local and national policies can negatively affect management proficiency. This tension is reflected by the National Audit Office (2011), which highlights additional variation between trusts in resource deployment and performance measurement, and limited sharing of best practice.
The Keogh Review (NHS England 2013) demonstrates how variation in service management can lead to patient confusion, significantly reducing appropriate help-seeking behaviour. It is apparent that national standardisation of service management across ambulance trusts may improve how patients access urgent services. In addition, improving training and resource support for responding clinicians may also significantly increase use of referral pathways.
Discussion
An unexpected finding of this review was the distinct lack of clear definitions outlining what constitutes avoidable attendance and inappropriate use of services. A significant number of articles did not establish how appropriateness was measured, and those that did relied almost exclusively on retrospective opinion. Few articles subsequently highlighted rationales for concluding that patient behaviour was inappropriate, and those that did mostly presented their rationales narratively through interview extracts (Agarwal et al, 2011; Booker, Simmonds and Purdy 2013).
Booker, Simmonds and Purdy (2013) argue that appropriateness is almost always defined retrospectively by the healthcare professional, which would certainly explain why such a paucity of objective definitions exists. Furthermore, as demonstrated in this review, a significant number of factors exclusive to individual patients can influence help-seeking behaviour. In this respect, appropriateness is also defined subjectively by the patient. Jones (2011) suggests that healthcare providers should seek to improve care options rather than attempt to influence patient help-seeking behaviour. Perhaps services should therefore aim to educate patients through targeted campaigns, whilst simultaneously seeking to better understand patient requirements, and align services accordingly.
Similarly, few articles outlined how admission avoidance was defined. Coates (2013) was the only study that explored this in detail, and outlined that non-conveyance of a patient might not necessarily result in an avoided hospital admission, either due to inadequate use of referral pathways or subsequent medical need. This review has highlighted a universal lack of clarity regarding how successful admission avoidance is measured, and since this assessment is pivotal in evaluating adequate use of pathways, further clarity should be sought by ambulance services.
Conversely, almost all material discussing frequent users provided clear definitions of what was considered frequent use of services (Dent, Hunt & Webster 2010; Smith & McNally 2014; Scott et al, 2013; Edwards et al, 2014).
Several factors influencing patient behaviour in the context of inappropriate use were identified. A number of articles highlighted risk-averse behaviours by both patients and carers when dealing with minor illnesses due to misconceptions of condition urgency. In relation to chronic illnesses, patients demonstrated a reluctance to temporise symptoms, and often sought out the most immediate form of assistance. Material suggested that these behaviours were driven by misconceptions over the seriousness of conditions, in addition to a perceived lack of available alternatives.
Sanctioning of help-seeking behaviours by carers and relatives was an additional reoccurring theme, and interpersonal influence was found to exacerbate inappropriate use in most circumstances. Reviewed material demonstrates that patient education, whilst an important consideration, only accounts for a partial driver of patient behaviour. A large percentage of influence can be attributed to patients’ perception of barriers to alternative care. Strategies to reduce inappropriate use should aim to improve patient access to alternative care, whilst also improving education and raising awareness of community services.
It is well established that areas of social deprivation and poorer demographics suffer with increased health issues (National Institute for Health and Care Excellence 2012; Royal College of Nursing 2012), and this review furthermore found significant evidence to suggest that patients in this demographic may also significantly contribute towards inappropriate use (Agarwal et al, 2011; Association of Ambulance Chief Executives 2011; Scott et al, 2013; O’Cathain et al, 2013; Edwards et al, 2014; Smith & McNally 2014). Whilst the individual clinician should take caution in stereotyping patients, the implications for wider healthcare services in response management and healthcare promotion appear to be evident.
In relation to healthcare access, two dichotomous issues provide equal contribution to inappropriate use of emergency services. A perceived barrier to community care services was a reoccurring theme throughout a significant number of articles (Agarwal et al, 2011; Booker, Simmonds & Purdy 2013). This was combined inversely with the ease of access to ‘999’ and ED services, as well as unanimously positive patient experience using these services. It was furthermore suggested that barriers to non-urgent community care were not limited to patients. A number of articles highlighted that prehospital clinicians often encountered problems when attempting to refer patients unsuitable for A&E transport (NHS England 2013; O’Hara et al, 2014).
Whilst barriers to GP services were not explored in detail in this review, there is reasonable evidence suggesting that demand for these services is also increasing in line with other urgent and emergency care services (NHS England 2013). A review of current community care paradigms in the UK could be beneficial in establishing whether or not reform is required to meet evolving patient needs. There has been recent political suggestion that a solution may be found by bringing OOH care into the direct control of ambulance trusts (Roberts 2015).
The importance of multidisciplinary collaboration was emphasised universally across the majority of articles. Fragmentation of healthcare services was unanimously highlighted as a significant contributor to inappropriate ED attendance. There appears to be national inconsistency in the availability of alternative services (O’Hara et al, 2014), in addition to variation in prehospital awareness of available resources (National Audit Office 2011; O’Hara et al, 2014). The National Audit Office (2011) highlights that ambulance trusts are inconsistent in keeping directories of available referral pathways.
There is sufficient evidence to suggest a significant lack of collaboration, both between multidisciplinary services and between local trusts (NHS England 2013; Edwards 2014). Since this fragmentation affects so many factors of appropriate use, including patient and clinician behaviour and organisational management, it is reasonable to consider this to be the most significant finding of this review. Further research into the causes of systemic healthcare fragmentation, and proposals for reform should be considered of the utmost importance in addressing increasing demand and appropriate use of NHS services.
Internal healthcare factors were not limited to issues accessing alternative pathways. Service culture and clinical behaviours were also found to significantly contribute to inappropriate use of services (NHS England 2013; Newton et al, 2013; O’Hara et al, 2014). Oversensitive triage was observed at multiple stages of assessment, due to a combination of organisational and educational factors. Oversensitive telephone triage was also highlighted as a potential contributor to inappropriate ambulance dispatch (Turner et al, 2013).
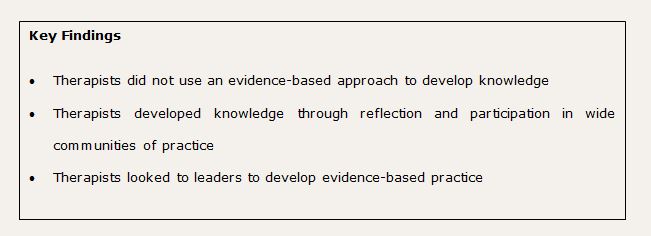
Studies showed that clinicians with greater experience, and specialised training, demonstrated greater levels of confidence in utilising referral pathways, and subsequently lower levels of over-triage. If the ambulance service is to continue along its current trajectory establishing itself as a signposting service (National Audit Office 2011), further investment must be made in specialised clinical roles and education of staff at all hierarchal levels. Established literature suggests that specialised prehospital roles are still nationally inconsistent (National Audit Office 2011; O’Hara et al, 2014), and standardisation would be beneficial in realising their full potential.
Conclusion
Appropriate usage is a poorly defined concept in healthcare, and whilst it may be argued that appropriateness is a subjective term, rationales for defining users as inappropriate are consistently omitted. Healthcare services cannot expect to observe appropriate use of channels without clarification of what this looks like. Further effort should be made to provide objective guidance to both patients and clinicians.
Patient education and socioeconomic status contributed to patient help-seeking behaviour. However, healthcare access and framework issues influenced much of this behaviour. Perceived and tangible barriers to healthcare, combined with situations of perceived urgency, prompted the use of more immediate healthcare channels, contributing heavily to inappropriate use. This was reflected in prehospital clinicians making conveyance decisions. Articles suggested that lack of confidence and organisational support also prompted disproportionately risk-averse behaviour from ambulance staff.
Fragmentation of multidisciplinary services was a superordinate and reoccurring theme throughout this study. In this respect this review has demonstrated the fundamental link, not just between ambulance and ED services, but also between all multidisciplinary healthcare services. Since many patients have a diverse and complex range of healthcare requirements (Knowles, O’Cathain & Nicholl 2010; Edwards et al, 2014), service providers are dependant on one another to ensure that users travel adequately and appropriately through channels. This review demonstrates that no single service can thrive in isolation, and that the collaboration of collective services is the most fundamental aspect of improving health services and the way patients access them. Whilst success is dependant upon the collective effort of wider multidisciplinary services, this review has shown the ambulance service to be in an ideal position to influence how patients access care, and how services interact with one another.
Edward Liscott, former Paramedic Practice BSc(Hons) student
References
Agarwal, S., J. Banerjee, R. Baker, S. Conroy, R. Hsu, A. Rashid, J. Camosso-Stefinovic, P. Sinfield and M. Habiba. 2011. Potentially avoidable emergency department attendance: interview study of patients’ reasons for attendance. Emergency Medicine Journal 29(3) [Online] Available From: http://emj.bmj.com.ezproxy.brighton.ac.uk/content/29/12/e3.full.pdf+html [13 April 2015]
Association of Ambulance Chief Executives. 2011. Taking Healthcare to the Patient 2: A review of 6 years’ progress and recommendations for the future. Association of Ambulance Chief Executives
Atenstaedt, R., S. Humphreys, H. Jones, and J. Newman. 2014. Choose Well: Reducing ‘inappropriate’ emergency department attendances. British Journal of Healthcare Management 20(8):392-395
Aveyard, H. 2014. Doing A Literature Review In Health And Social Care: A Practical Guide. 3rd ed. Maidenhead: Open University Press
BBC. 2015. NHS Winter 2014-15: Weekly A&E tracker. [Online] BBC. Available From: http://www.bbc.co.uk/news/health-25055444 [26 April 2015]
Booker, M., R. Simmonds and S. Purdy. 2013. Patients who call emergency ambulances for primary care problems: a qualitative study of the decision-making process. Emergency Medicine Journal 0:1-5 [Online] Available From: http://emj.bmj.com/content/early/2013/03/26/emermed-2012-202124.full.pdf+html [7 April 2015]
Brunton, G., C. Stansfield and J. Thomas. 2012. Finding Relevant Studies. In: An Introduction to Systematic Reviews, edited by D. Gough, S. Oliver and J. Thomas. London: SAGE
Coates, D. 2013. ECPs: avoiding emergency department attendance or hospital admission? Journal of Paramedic Practice 2(4):158-168
Colver, K., P. Abhyankar and C. Niven. 2015. Ambulance service treat and refer guidelines: a qualitative investigation into the use of treat and refer guidelines by ambulance clinicians. Emergency Medicine Journal 32(5):e1-e11
Cooper, C. 2015. NHS A&E crisis: Hospitals struggle to keep up with festive demand. [Online] The Independent. Available From: http://www.independent.co.uk/news/uk/politics/nhs-ae-crisis-hospitals-struggle-to-keep-up-with-festive-demand-9954833.html [26 April 2015]
Dent, A., G. Hunt and A. Webster. 2010. The Impact of frequent attenders on a UK emergency department. European Journal of Emergency Medicine 17(6):332-336
Department of Health. 2005. Taking Healthcare to the Patient: Transforming NHS Ambulance Services. London: DH
Department of Health and Ageing. 2007. Emergency Triage Education Kit Triage Workbook. Canberra: Commonwealth of Australia Department of Health and Ageing
Donohoe, R. and A. Blaber. 2008. Professional Issues Affecting Practice. In: Foundations For Paramedic Practice, edited by A. Blaber. Maidenhead: Open University Press
Eastwood, K., A. Morgans, K. Smith and J. Stoelwinder. 2014. Secondary triage in prehospital emergency ambulance services: a systematic review. Emergency Medicine Journal 0:1-7 [Online] Available From: http://emj.bmj.com/content/early/2014/04/30/emermed-2013-203120.full.pdf+html [1 May 2015]
Edwards, M., G. Bassett, L. Sinden and R. Fothergill. 2014. Frequent callers to the ambulance service: patient profiling and impact of case management on patient utilisation of the ambulance service. Emergency Medicine Journal 0:1-5 [Online] Available From: http://emj.bmj.com/content/early/2014/10/13/emermed-2013-203496.full [4 April 2015]
Edwards, N. 2014. Community services: How they can transform care. London: The King’s Fund
Endacott, R., S. Cooper, R. Sheaff, J. Padmore and G. Blakely. 2010. Improving emergency care pathways: an action research approach. Emergency Medicine Journal 28(3):203-207
Francis, R. 2013. Report of the Mid Staffordshire NHS Foundation Trust Public Inquiry. London: The Stationery office.
GRADE Working Group. 2004. Grading quality of evidence and strength of recommendations. BMJ 328(7454):1490-1494
Halter, M., S. Vernon, H. Snooks, A. Porter, J. Close, F. Moore and S. Porsz. 2011. Complexity of the decision-making process of ambulance staff for assessment and referral of older people who have fallen: a qualitative study. Emergency Medicine Journal 28(1):44-50
House of Commons. 2004. GP Out-of-Hours Services: Fifth Report of Session 2003–04. London: The Stationery Office
Johnston, I. 2015. Ambulance staff told to leave patients at A&E departments if they have not been admitted after 45 minutes. [Online] The Independent. Available From: http://www.independent.co.uk/life-style/health-and-families/health-news/ambulance-staff-told-to-leave-patients-at-ae-departments-if-they-have-not-been-admitted-after-45-minutes-9986678.html [26 April 2015]
Jones, D. 2011. How GPs can help reduce inappropriate attendance. Emergency Nurse 19(4):20-23
Kirkby, H. and L. Roberts. 2011. Inappropriate 999 calls: an online pilot survey. Emergency Medicine Journal 29(2):141-146
Knowles, E., A. O’Cathain and J. Nicholl. 2010. Patients experiences and views of an emergency and urgent care system. Health Expectations 15(1):78-86
Kyle, R., M. Banks, S. Kirk, P. Powell and P. Callery. 2013. Avoiding inappropriate paediatric admission: facilitating General Practitioner referral to Community Children’s Nursing Teams. BMC Family Practice 14(4):1-8 [Online] Available From: http://www.biomedcentral.com/1471-2296/14/4 [27 April 2015]
Lavrakas, P. 2008. Encyclopedia of Survey Research Methods. London: SAGE
LoBiondo-Wood, G. & J. Haber. 2013. Nursing Research: Methods and Critical Appraisal for Evidence-Based Practice. 8th ed. Missouri: Mosby
Local Ambulance Trust. 2015. Immediate Handover – Standard Operating Procedure. Local Ambulance Trust
Machi, L. and B. McEvoy. 2009. The Literature Review. London: SAGE
MAG Online Library. 2014. Healthcare and education content from the Mark Allen Group. [Online] Mark Allen Group. Available From: http://www.magonlinelibrary.com/ [3 April 2015]
Mani, S., D. Bertfield, A. Ritchie, A. Webber and C. Lisk. 2014. Emergency admission prevention: data from 619 patients referred to a new community based admissions avoidance scheme integrating health and social care. Age and Ageing 43(2):ii1
May, T. 2011. Social Research: Issues, Methods and Process. 4th ed. Maidenhead: Open University Press
Moher, D., A. Liberati, J. Tetzlaff and D. Altman. 2009. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med 6(7):1-6
Morris, P. 2009. Leading the way in clinical effectiveness. Journal of Paramedic Practice 1(7):299-301
Mundasad, S. 2014. Patients ‘face long queues in ambulances outside A&E’. [Online] BBC. Available From: http://www.bbc.co.uk/news/health-28706796 [26 April 2015]
National Audit Office. 2011. Transforming NHS ambulance services. London: The Stationary Office
National Institute for Health and Care Excellence. 2006. Methods for development of NICE public health guidance. London: NICE
National Institute for Health and Care Excellence. 2012. Health inequalities and population health. [Online] NICE. Available From: https://www.nice.org.uk/advice/lgb4/chapter/What-NICE-says [6 May 2015]
National Institute for Health and Care Excellence. 2015. Healthcare Databases. [Online] NICE. Available From: http://www.library.nhs.uk/hdas [3 April 2015]
Nelson, J. 2011. Why patients visit emergency units rather than use primary care services. Emergency Nurse 19(1):32-36
Newton, M., E. Tunn, I. Moses, D. Ratcliffe and K. Mackway-Jones. 2013. Clinical navigation for beginners: the clinical utility and safety of the Paramedic Pathfinder. Emergency Medicine Journal 0:1-6 [Online] Available From: http://emj.bmj.com/content/early/2013/10/07/emermed-2012-202033.full.pdf+html?hwoasp=authn%3A1428508209%3A4223626%3A1534939456%3A0%3A0%3AHrY2%2F7J85Q1Wi%2B4fF%2BCCNg%3D%3D [7 April 2015]
NHS England. 2013. High quality care for all, now and for future generations: Transforming urgent and emergency care services in England The Evidence Base from the Urgent and Emergency Care Review. NHS England
NHS England. 2015. Risk Management Policy and Process Guide. NHS England
NHS Office of Strategic Health Authorities. 2008. Emergency Service Review: Good Practice Guide for Ambulance Services and their Commissioners. London: Office of Strategic Health Authorities.
O’Brien, G., M. Shapiro, R. Woolard, P. O’Sullivan and M. Stein. 1996. “Inappropriate” Emergency Department Use: A Comparison of Three Methodologies for Identification. Academic Emergency Medicine 3(3):252-257
O’Cathain, A,. E. Knowles, R. Maheswaran, T. Pearson, J. Turner, E. Hirst, S. Goodacre and J. Nicholl. 2013. A system-wide approach to explaining variation in potentially avoidable emergency admissions: national ecological study. BMJ Quality and Safety 23(1):47-55
O’Hara, R., Maxine Johnson, A. Siriwardena, A. Weyman, J. Turner, D. Shaw, P. Mortimer, C. Newman, E. Hirst, M. Storey, S. Mason, T. Quinn and J. Shewan. 2014. A qualitative study of systemic influences on paramedic decision making: care transitions and patient safety. Journal of Health Services Research & Policy 20(1):45-53
O’Hara, R., M. Johnson, E. Hirst, A. Weyman, D. Shaw, P. Mortimer, C. Newman, M. Storey, J. Turner, S. Mason, T. Quinn, J. Shewan and A. Siriwardena. 2015. Decision making and safety in ambulance service transitions. Emergency Medicine Journal 32(5):e1-e11
Pannucci, C. and E. Wilkins. 2010. Identifying and Avoiding Bias in Research. Plastic and Reconstructive Surgery 126(2):619-625
Patton, G. and S. Thakore. 2012. Reducing inappropriate emergency department attendances: a review of ambulance service attendances at a regional teaching hospital in Scotland. Emergency Medicine Journal 30(6):459-461
Press Association. 2013. Pressure on A&E departments is out of control, warns NHS regulator. [Online] Guardian News. Available From: http://www.theguardian.com/society/2013/may/09/demand-a-and-e-out-of-control [26 April 2015]
Raleigh, V. and F. Frosini. 2012. Improving GP services in England: exploring the association between quality of care and the experience of patients. The King’s Fund
Ridley, D. 2012. The Literature Review: A Step-by-Step Guide for Students. 2nd ed. London: SAGE
Roberts, N. 2015. GP out-of-hours could integrate with ambulances and 111 under Labour. [Online] Haymarket Media Group. Available From: http://www.gponline.com/gp-out-of-hours-integrate-ambulances-111-labour/article/1331237 [6 May 2015]
Royal College of Nursing. 2012. Health inequalities and the social determinants of health. London: Royal College of Nursing
Scott, J., A. Strickland, K. Warner and P. Dawson. 2013. Frequent callers to and users of emergency medical systems: a systematic review. Emergency Medicine Journal 31(8):684-691
Smith, D. and A. McNally. 2014. Delivering enhanced safety, productivity and experience: early results from a frequent caller management system. Journal of Paramedic Practice 6(12):634-641
Snooks, H., W. Cheung, J. Close, J. Dale, S. Gaze, I. Humphreys, R. Lyons, S. Mason, Y. Merali, J. Peconi, C. Phillips, J. Phillips, S. Roberts, I. Russell, A. Sánchez, M. Wani, B. Wells, and R. Whitfield. 2010. Support and Assessment for Fall Emergency Referrals (SAFER 1) trial protocol. Computerised on-scene decision support for emergency ambulance staff to assess and plan care for older people who have fallen: evaluation of costs and benefits using a pragmatic cluster randomised trial. BMC Emergency Medicine 10(2):1-8
South East Coast Ambulance Service. 2015. Stroke Awareness. [Online] South East Coast Ambulance Service. Available From: http://www.secamb.nhs.uk/get_involved/health_campaigns/stroke_awareness.aspx [7 May 2015]
Steckler, A. and. McLeroy. 2007. The Importance of External Validity. American Journal of Public Health 98(1):9-10
Thomas, J., A. Harden and M. Newman. 2012. Synthesis: Combining results systematically and appropriately. In: An Introduction to Systematic Reviews, edited by D. Gough, S. Oliver and J. Thomas. London: SAGE Publications Ltd.
Turner, J., A. O’Cathain, E. Knowles and J. Nicholl. 2013. Impact of the urgent care telephone service NHS 111 pilot sites: a controlled before and after study. BMJ Open 3(11):1-8 [Online] Available From: http://bmjopen.bmj.com/content/3/11/e003451.full.pdf [7 April 2015]
University of Sheffield Medical Care Research Unit. 2010. Building the evidence base in pre-hospital urgent and emergency care: a review of research evidence and priorities for future research. London: DH
Watters, P. 2014. Literature Searching. [PowerPoint] University of Brighton. Brighton: University of Brighton
Whitnell, J. 2008. Psychology: an introduction. In: Foundations For Paramedic Practice, edited by A. Blaber. Maidenhead: Open University Press
 The hospital Trust has gained confidence in the merits of involving student volunteers and more projects and new collaborations have since been generated. Students add value to bespoke projects that otherwise might not have taken place. Students have referred to their volunteering experiences at employment interviews and reported favourable responses.
The hospital Trust has gained confidence in the merits of involving student volunteers and more projects and new collaborations have since been generated. Students add value to bespoke projects that otherwise might not have taken place. Students have referred to their volunteering experiences at employment interviews and reported favourable responses.